The healthcare setting often involves sensitive and intimate exams that present challenges other businesses don’t face. Medical chaperones can provide a level of comfort for patients and may help ensure the best possible experience for patients and physicians alike. In so doing, the likelihood of a sexual misconduct allegation based on a misunderstanding is greatly reduced.1 And while the case study below involves a physician and this article references physicians throughout, the lessons and recommendations are applicable to any healthcare professional.
Download the InfographicRecognizing the sensitive nature of the clinical encounter, the AMA Code of Medical Ethics makes it the responsibility of physicians to respect the dignity of their patients by providing “a comfortable and considerate atmosphere for the patient and the physician.” Part of this effort, it goes on to say, includes providing gowns, privacy for undressing, and sensitive use of draping for patients, but it also includes making medical chaperones available.2
Utilizing Medical Chaperones in Your Practice
Physical touch, discussion of sensitive health conditions, and procedures of an intimate nature are a routine part of the physician-patient encounter. A medical chaperone is a member of the healthcare team present (with patient consent) during the physician-patient encounter who can help reassure or comfort patients during examinations, thereby reducing the likelihood of an allegation of sexual misconduct that’s based on a misunderstanding.1 The use of a chaperone can apply even in some behavioral therapy settings when a physical assessment is performed to evaluate medical health, according to the American Psychiatric Association’s Practice Guidelines.3
Even with chaperones, though, misunderstandings of behavior are still possible. For this reason, it is important to document both the presence of the chaperone and their full name and job title in the patient record.
NORCAL Closed Claim Case Study: OB/GYN and Patient
A patient established care with an OB/GYN and requested to have an IUD inserted. Medical records from previous providers indicated that she had an unremarkable gynecological history and was a suitable candidate for placement of an IUD. The procedure, which seemed to go well, was performed by a male OB/GYN. There was no chaperone present during the exam and procedure. The patient was advised to make a follow‐up appointment for an ultrasound to confirm correct IUD placement.
During the ultrasound at her follow-up appointment, the patient became agitated and distraught. She revealed to the female ultrasound tech that she does not remember everything about the IUD insertion by the doctor at her previous visit and that she believes he raped her during the procedure. At the conclusion of the ultrasound, the tech reported the patient’s statements to clinic administration. The patient subsequently filed a sexual misconduct claim against the OB/GYN and the clinic.
Assuming nothing untoward occurred, this case is an excellent example of how a medical chaperone could have provided comfort to the patient during the procedure and protected the physician by providing a witness afterward to what transpired.
Medical Liability Risk Management Recommendations
 Providing the “comfortable and considerate atmosphere for the patient and the physician” called for in the AMA Code of Medical Ethics2 requires a multi-faceted approach, including making medical chaperones available and establishing and maintaining boundaries of appropriate behavior. Healthcare providers should also establish and communicate a sexual misconduct policy that details these efforts and the proper response when allegations are raised, as demonstrated by the ultrasound tech in the above case.
Providing the “comfortable and considerate atmosphere for the patient and the physician” called for in the AMA Code of Medical Ethics2 requires a multi-faceted approach, including making medical chaperones available and establishing and maintaining boundaries of appropriate behavior. Healthcare providers should also establish and communicate a sexual misconduct policy that details these efforts and the proper response when allegations are raised, as demonstrated by the ultrasound tech in the above case.
Best Practices for Using Medical Chaperones1
The following best practices can help educate staff on the use of medical chaperones and help your practice develop a medical chaperones policy.
- Develop a chaperone policy to guide staff in determining which patient encounters should involve the use of a chaperone and ensure that all providers and staff are aware of the policy.
- Clearly define the role of a chaperone.
- Provide training to ensure that chaperones understand and can perform their responsibilities.
- Discourage the use of family members as chaperones. Include a designated chaperone from the practice even if a family member is present during the examination.
- Offer a separate opportunity for private conversation between the physician and patient.
- Document the chaperone’s presence during the exam, including full name and job title.
- Identify situations when an examination can take place without a chaperone if a patient refuses one and when alternative arrangements are needed. Document the refusal of a chaperone.
- In keeping with AMA guidance, limit sensitive inquiries and history taking during a chaperoned examination.2
- Regularly review the chaperone policy to ensure that it remains relevant and up-to-date.
Chaperone use is only one aspect of guarding against sexual misconduct allegations. The following recommendations can further help to provide a safe and comfortable environment for physician and patient alike and ensure the best therapeutic outcome for the patient.
Establish and Maintain Boundaries of Appropriate Behavior1
Because physicians listen empathetically to their patients’ problems during clinical encounters and attempt to help them, a patient can sometimes see their physician as a friend and may exhibit transference behavior and project reciprocal feelings onto the physician, perceiving that the two have a mutual intimate relationship. Physicians, likewise, can occasionally blur these boundaries, either intentionally or unintentionally. In any physician-patient relationship, therefore, it is important to establish and maintain appropriate boundaries consistent with the basic principles of medical ethics to ensure that a professional relationship is fostered and maintained.
- Recognize early signs when the patient verbally expresses or exhibits behavior that endangers the professional relationship and determine appropriate steps to bring the relationship back into compliance.
- Do not make statements or exhibit behavior that contributes to the blurring of boundaries or that could be misconstrued and misinterpreted by the patient. Thoroughly document all professional patient encounters.
- If a patient exhibits inappropriate behavior, respond immediately by setting proper boundaries to prevent misunderstandings. Document the patient’s behavior and your response.
- Be compassionate but firm when it comes to recognizing and addressing inappropriate behaviors exhibited by patients.
- Consult with a colleague when unsure about how to address inappropriate patient behavior.
- Do not be in denial or give the patient the benefit of the doubt if you perceive that the patient is being manipulative through inappropriate words and behavior.
- Appropriately terminate the physician-patient relationship when it is clear that an appropriate professional relationship cannot be maintained.
Establish a Sexual Misconduct Policy1
Developing and communicating a sexual misconduct policy is essential to all healthcare providers.
- Include information regarding acceptable and unacceptable professional interactions with patients, including, but not limited to, sexual misconduct.
- Provide in‐service training to educate providers and staff about the policy.
- Orient new providers to the policy and regularly review the policy with current providers.
- Ensure that all providers set and maintain professional boundaries in provider-patient interactions.
- Advise providers and staff to avoid any flirtatious behavior (or behavior that could be construed or perceived as flirtatious) toward patients.
- Allow all patients to disrobe and dress in private whenever possible.
- Provide a gown or appropriate drape to cover exposed areas.
- Educate patients about the reasons and methods for the examination, especially for sensitive and intimate exams.
- Include clear procedures for how to proceed if a patient alleges sexual misconduct, including:
- Assure the patient that you are taking their concerns seriously and that the matter will be investigated in an appropriate manner.
- Contact your professional liability carrier immediately for guidance and coverage determinations.
- Contact your personal or business attorney for additional guidance.
- Limit communications about the incident to appropriate individuals on a need-to-know basis.
- If the patient makes statements about the incident in public forums such as social media or ratings websites, do not challenge the patient or defend yourself. This could complicate the defense of any claims and may also violate HIPAA privacy guidelines.
Article References
1. NORCAL Group Risk Management CME webinar, “Professionalism and Utilization of Medical Chaperones: Avoiding Allegations of Familiarity/Sexual Impropriety.”
2. American Medical Association. “Use of Chaperones: Code of Medical Ethics Opinion 1.2.4.” (accessed 6/6/2019)
3. American Psychiatric Association. “Guideline VI. Assessment of Medical Health.” Practice Guidelines for the Psychiatric Evaluation of Adults, Third Edition. (accessed 6/6/2019)
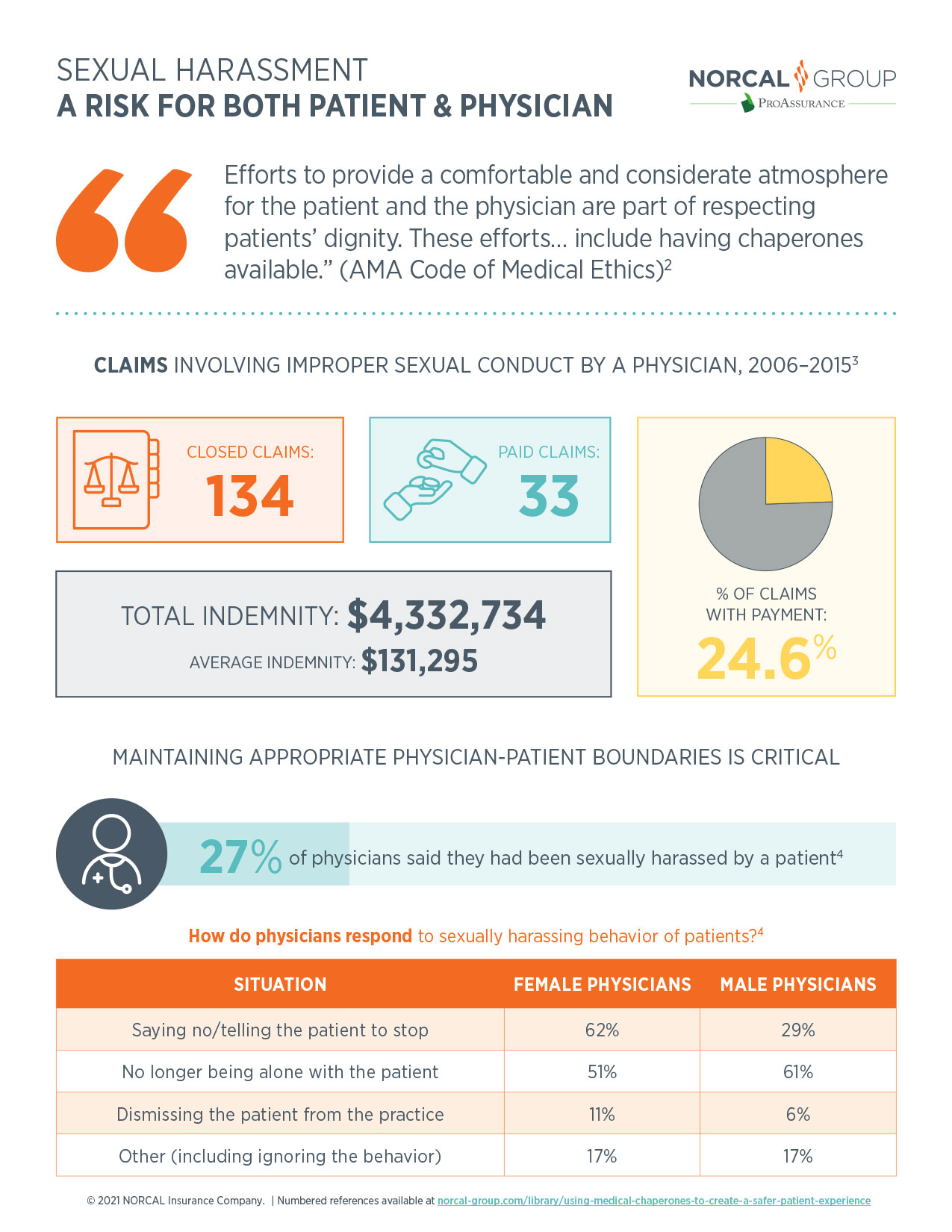
Infographic References
1. NORCAL Group Risk Management CME webinar. “Professionalism and Utilization of Medical Chaperones: Avoiding Allegations of Familiarity/Sexual Impropriety.” 10/10/2018.
2. American Medical Association. “Use of Chaperones: Code of Medical Ethics Opinion 1.2.4.” (accessed 6/6/19)
3. Medical Professional Liability Association (MPL) Data Sharing Project. Sexual misconduct allegations and claims data (2006–2015) as reported by member carriers, including NORCAL Group companies. Used with permission.
4. Leslie Kane. “Patients Sexually Harassing Physicians: Report 2018.” Medscape, 7/11/2018. (accessed 6/6/2019)

